~ The following is a press release provided by the University of Florida. It has been published here as received, without additional reporting or editing by Alachua County Today staff. ~
GAINESVILLE, Fla. — UF Health Cancer Center researchers have found a surprising culprit behind common health problems like obesity, diabetes and fatty liver disease: silent genetic glitches in the blood system that occur naturally as people age.
The findings, published in the Journal of Clinical Investigation, mean that in the future, simple blood tests could be developed to identify people most at risk early on, helping prevent chronic illnesses and cancer through strategies like diet or lifestyle changes.
“Most people don’t think about the blood as causing obesity and related diseases, but our surprising findings highlight that there’s a causal relationship between mutations in blood stem cells and metabolic diseases,” said lead author Bowen Yan, Ph.D., a research assistant professor in the Department of Pharmacology and Therapeutics in the UF College of Medicine.
As people age, stem cells in the bone marrow that produce blood cells gradually accumulate mutations in their DNA. Most mutations don’t cause any issues, but sometimes blood stem cells with a mutation can start crowding out their peers. Called clonal hematopoiesis, this condition affects about 10% of older people and is associated with an increased risk of blood cancers like leukemia.
Clonal hematopoiesis is linked to a higher risk of obesity and diabetes, studies using large databases of patient records like the UK Biobank and the National Institutes of Health’s All of US Research Program have shown. But the prevailing thinking was that obesity and related conditions promoted blood cell changes, not the other way around. The new study reverses that.
“We found that blood cell mutations don’t just show up because of poor health — they can cause it,” Yan said.
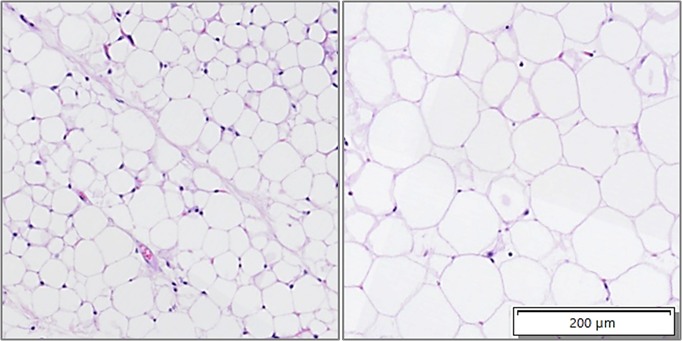
As part of their study, the researchers put a genetic mutation commonly involved in clonal hematopoiesis into the blood system of otherwise healthy mice. Mice with the mutation started to eat more and gained weight more rapidly than those without the mutation. They developed high blood sugar and were more prone to liver problems.
The effects were even stronger when mice were fed a high-fat, high-sugar “Western” diet — nutritionally similar to a Big Mac, French fries and milkshake diet: Their weight exploded.
“Mutations in the blood system are driving these conditions,” said senior author Olga Guryanova, Ph.D., an associate professor in the Department of Pharmacology and Therapeutics. “Clonal hematopoiesis is usually a silent condition, but if you know you have it, you’re better aware of the risks it’s associated with. Our hope is that knowing these risk factors would allow us to manage chronic conditions more efficiently, either with drugs or personalized lifestyle and diet interventions.”
The implications could be far-reaching, particularly as obesity has now overtaken smoking as the most significant and preventable risk factor for cancer.
“With the ability to predict the risk of obesity and metabolic disease and better manage it, we could also eventually mitigate the risk of developing cancer,” Guryanova said.
The team is studying how the mutations drive disease. Next, they plan to test how drugs like those commonly used to treat diabetes and new popular weight loss drugs might help reverse or prevent diseases caused by blood cell changes.
Researchers from Queen’s University in Canada contributed. The study received funding from the National Institutes of Health, American Cancer Society, Edward P. Evans Foundation, Oxnard Family Foundation, Ocala Royal Dames for Cancer Research and UF Health Cancer Center, where both Yan and Guryanova are members.
# # #
email editor@
alachuatoday.com
Study Finds Hidden Blood Mutations Spark Obesity, Diabetes and Liver Disease
Tools
Typography
- Font Size
- Default
- Reading Mode